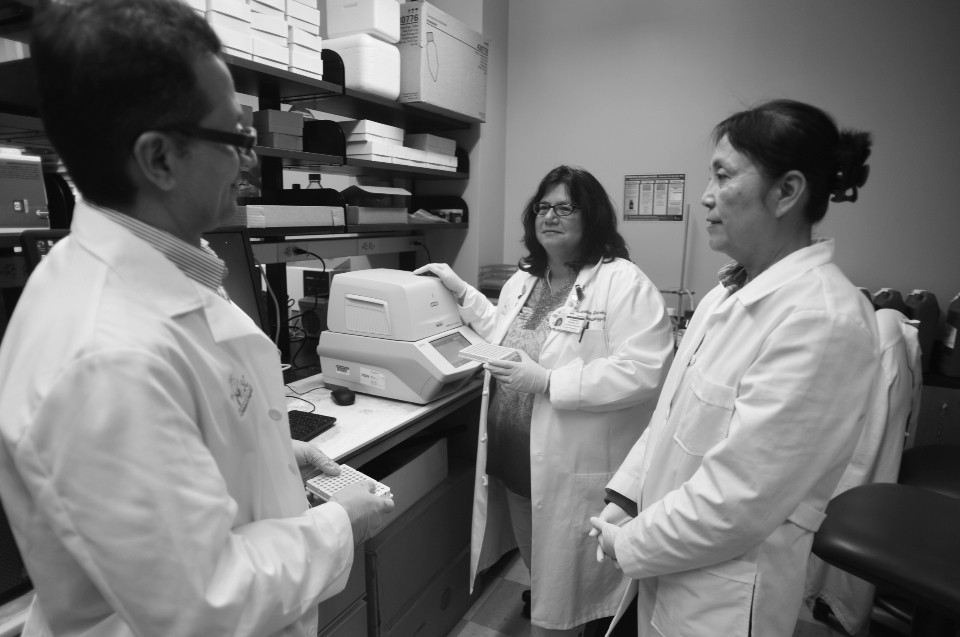
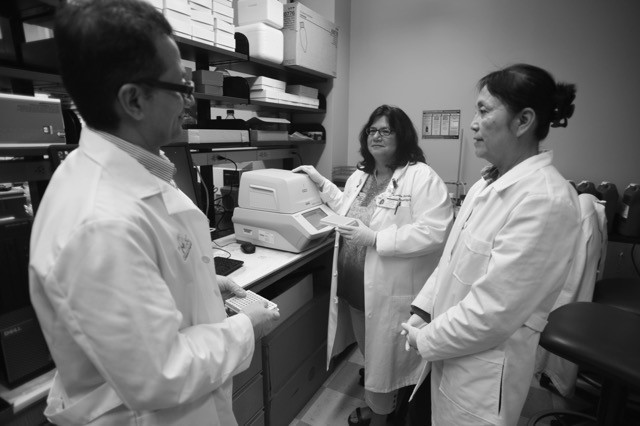
Chase After a Cure supports a research laboratory at the Medical University of South Carolina (MUSC) that’s at the forefront of pediatric cancer research today. Our organization has been paying the lion’s share of the lab’s expenses in recent years, raising close to a million dollars since 2008. During this time, the lab’s head Dr. Jacqueline Kraveka and the national research consortium she works with have made great strides in developing the research and furthering the clinical trials which will one day hopefully result in a cure.